Construction of Nipah Virus Vaccine
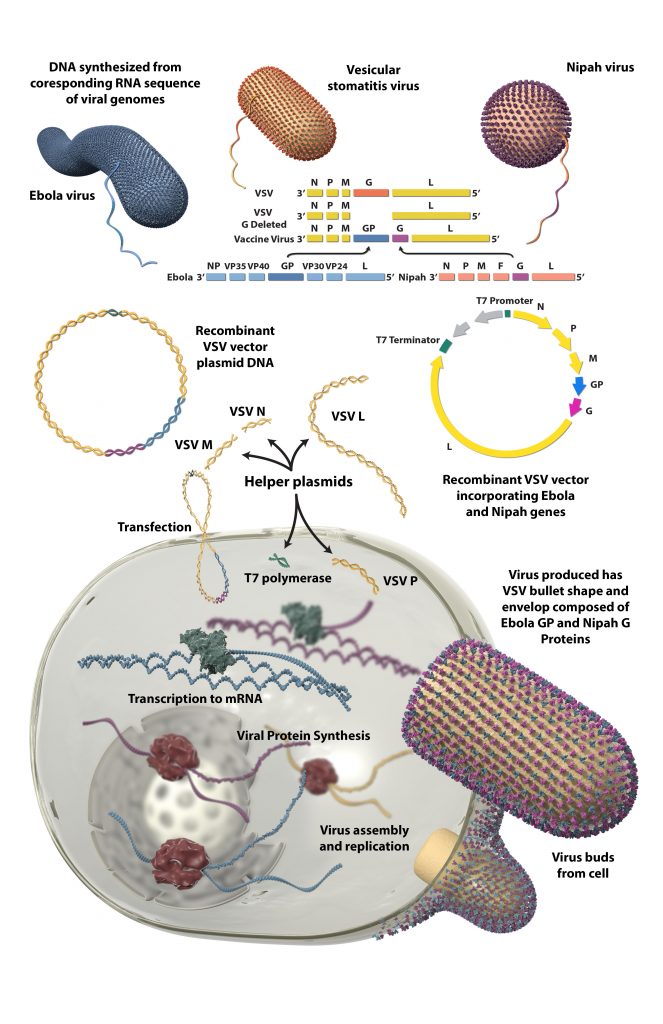
Construction of a synthetic virus. Our Nipah vaccine is created by chemical synthesis and molecular cloning, also known as recombinant DNA technology. The process (see figure) is referred to as ‘reverse genetics’, because it starts with known DNA sequences and produces a novel sequence (the vaccine virus).1In ‘regular genetics’, the DNA sequence is used or modified to produce a protein The Nipah vaccine starts with chemically synthesizing stretches of DNA corresponding to multiple genes from different viruses that, when stitched together, comprise a novel virus that does not occur in nature (a ‘chimera’2The word chimera derives from Greek mythology, referring to an animal composed of parts of another animal). The genetic sequences of parts of three different viruses are cloned using enzymes that cut and reassemble DNA into a full-length copy of the entire viral genome. The full-length purified DNA is then introduced into cells using synthetic lipids that complex to DNA and can fuse with the lipid in cell membranes, allowing entry into the cytoplasm of the cell (a process called ‘transfection’). Once inside the cell, the DNA serves as a template for copying complementary strands of RNA, facilitated by an enzyme (RNA polymerase), and, in turn, the RNA is translated into proteins and transcribed into new copies of RNA needed for replication and production of new virus particles. This synthetic process is self-sustaining, since the new virus particles are able to infect new cells, either in cell cultures for manufacturing, or in vivo when injected into humans or animals.
Composition of the Nipah vaccine. The Nipah vaccine is a chimera composed of genes from three different sources: Vesicular stomatitis (VSV), Ebola, and Nipah viruses. The safe and effective vaccine against Ebola, produced by Merck and approved for human use by the FDA, the European Medicines Agency, and the WHO, is a synthetic chimera of VSV and Ebola genes. Our new Nipah vaccine is similar in composition to the Ebola vaccine, but adds an additional gene encoding a protein (the Glycoprotein or “G” protein) of Nipah virus (Figure). The inclusion of the Ebola glycoprotein (GP) gene provides an important structural and functional component of the viral envelope needed for fusion to cell membranes and entry into cells. Four VSV genes form the backbone of the vaccine, and are required for replication of the virus in cells, whereas the Ebola GP forms the viral envelope; it is not yet proven if the Nipah G protein is incorporated in the viral envelope or is expressed in the infected cell without forming a structural component of the bullet-shaped virus particle.
Safety of the live, replicating, recombinant Nipah vaccine. Like many of the most successful vaccines used to protect against infectious diseases (e.g. measles, mumps, German measles, chickenpox, smallpox, oral polio, rotavirus, yellow fever), the recombinant vaccine against Nipah is a live, replication competent vaccine, engineered to balance safety and effectiveness. All three components of the vaccine (the VSV backbone, Ebola GP and Nipah G) are derived from viruses of animals. VSV causes a non-fatal disease in livestock (principally pigs, cattle, horses) characterized by blistering of mucous membranes. Humans may become infected with VSV but have either no overt disease or, infrequently, mild flu-like illness. Thus, VSV is already an attenuated virus with respect to human infection. Other features of the vaccine construct provide further safety features and attenuation. The envelope glycoprotein of VSV, which is responsible for virulence of the virus is deleted and replaced with foreign genes (from Ebola and Nipah). This process of ‘chimerization’ is well-known to significantly attenuate viruses by reducing both the quantity of new particles produced by cells and the dysfunction of cellular processes. The fact that the Nipah vaccine includes the Ebola GP, (also contained in the approved recombinant VSV Ebola vaccine), with the single addition of (Nipah G) protein, provides an additional level of confidence in its target product profile. In animal experiments conducted so far, the rVSV-Nipah vaccine appears to be very well tolerated (and protective) in animals (including nonhuman primates), but clinical trials have yet to be performed.
Stimulation of an immune response to Nipah. Because they replicate in the host, live attenuated vaccines can stimulate rapid onset immunity after a single dose. This is the case for the rVSV Ebola vaccine which induced protective immunity within 10 days after a single inoculation in two field trials.3Henao-Restrepo AM, Efficacy and effectiveness of an rVSV-vectored vaccine in preventing Ebola virus disease: final results from the Guinea ring vaccination, open-label, cluster-randomised trial (Ebola Ça Suffit!). Lancet. 2017 Feb 4;389(10068):505-518.4WHO. Preliminary results on the efficacy of rVSV-ZEBOV-GP Ebola vaccine using the ring vaccination strategy in the control of an Ebola outbreak in the Democratic Republic of the Congo: an example of integration of research into epidemic response. https://www.who.int/csr/resources/publications/ebola/ebola-ring-vaccination-results-12-april-2019.pdf (accessed 28 March 2020). When the recombinant VSV-Nipah vaccine virus is injected into the body, it replicates to produce new virus particles that infect millions of cells and produce Nipah G protein, the antigen against which an immune response is desired. A combination of factors in this process combine to stimulate a strong immune response against the Nipah virus. First, the G protein antigen contains specific molecular structures (‘epitopes’) that are preserved for recognition by the immune system, leading to production of antibodies, stimulation of T cells and immunological memory. Antibodies to the Nipah G epitopes are strongly neutralizing, i.e. capable of disabling and killing Nipah virus. Second, the initial virus replication rapidly stimulates multiple genes in the cells infected with the vaccine virus which, in response, produce chemical substances (cytokines), including interferon, that enhance the specific antibody and T cell responses.
Protection against Nipah virus disease. The principle of vaccination is to stimulate a lasting immune response, characterized typically by the generation of antibodies, that protects against infection on future exposure to the pathogen, in this case Nipah virus. The immune system incorporates mechanisms for immunologic memory, so that the vaccinated individual can recognize the antigen (virus) and rapidly and specifically recall the immune response; this feature is characteristic of live, attenuated vaccines that may provide durable, even lifelong immunity. Both neutralizing antibodies that directly disable the invading virus, and non-neutralizing antibodies that bind virus and interact with receptors on cells (e.g. macrophages, neutrophils, natural killer cells) play a role in protection. In animal models of Nipah virus disease, including hamsters and African green monkeys, immunization with the rVSV-Nipah vaccine candidate stimulated a strong antibody response and protected 100% of the animals against challenge with Nipah virus.5Prescott, J., et al., Single-dose live-attenuated vesicular stomatitis virus-based vaccine protects African green monkeys from Nipah virus disease. Vaccine, 2015;33(24): 2823-9.6DeBuysscher, B., et al., Peri-exposure protection against Nipah virus disease using a single-dose recombinant vesicular stomatitis virus-based vaccine. Npj Vaccines, 2016;1:16002;doi:10.1038/npjvaccines.201627DeBuysscher, B.L. et al., Single-dose live-attenuated Nipah virus vaccines confer complete protection by eliciting antibodies directed against surface glycoproteins. Vaccine, 2014;32(22):2637-44 The role of antibodies in the protective immune response was shown by transferring serum from vaccinated to unvaccinated hamsters and challenging the animals with Nipah virus; serum from immunized but not from normal control animals was fully protective.